A new diagnosis can feel overwhelming. You’re not alone—and small, repeatable actions make a big difference with Type 2 Diabetes. This guide shows how to track glucose, plan meals, reach ~150 minutes of weekly activity, and use devices and medications together so your levels stay in range more often.You may feel overwhelmed the moment you hear a chronic diagnosis, and that worry is real. But you are not alone, and small steps can change your day and your long-term health.
This guide will show practical, everyday actions for tracking blood sugar, planning meals, and fitting about 150 minutes of activity into a week so you can lower glucose and support weight goals.
You’ll learn how devices like a glucose meter or a continuous monitor fit your needs, plus how medications and lifestyle work together so your levels stay in range more often.
I also promise a clear review of supplements later, including a HepatoBurn Review, so you can separate safe, useful options from hype.
Key Takeaways
- You’ll get simple, daily steps for managing diabetes and monitoring blood regularly.
- Exercise, meal plans, and meds work together to help you keep sugar levels steady.
- Learn device options and how to choose between a meter and a CGM based on access and cost.
- Find sustainable lifestyle tips to lower overwhelm and support long-term care.
- Later sections include a supplements review, with a focused HepatoBurn Review for safety checks.
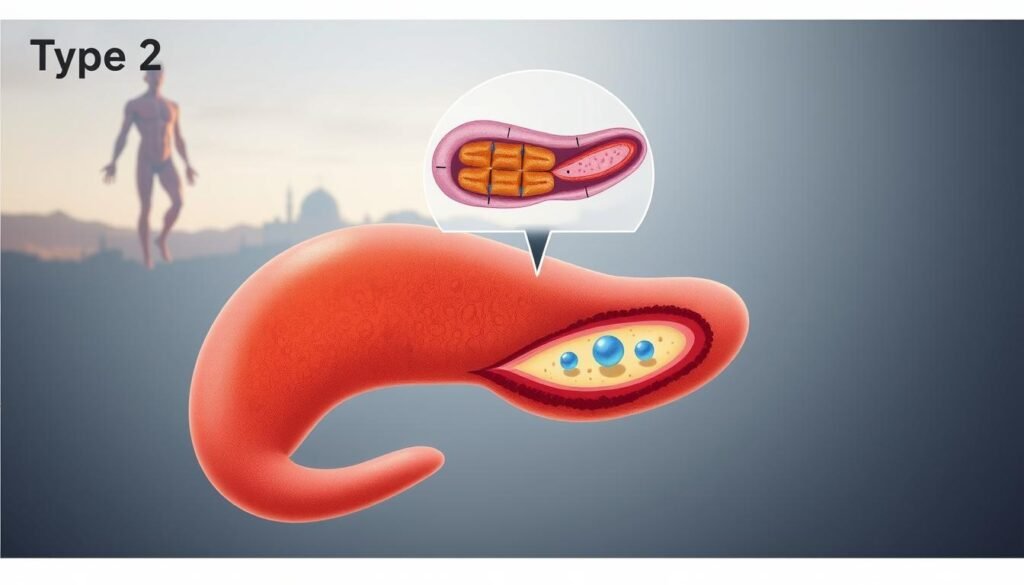
Type 2 diabetes at a glance: What it is and why management matters
Knowing what happens in your body when glucose rises makes management less mysterious and more practical.
Your body gets energy from glucose made when you eat. Insulin is the hormone that helps move that glucose into cells so you can use that energy.
When the body does not make enough insulin or does not use it well, blood sugar and blood glucose levels climb. Over time, high levels harm vessels and organs and raise risk of serious disease.
- Your body turns food into glucose for energy. Insulin moves glucose into cells.
- With Type 2 Diabetes, insulin is low and/or cells resist it → blood sugar rises.
- Consistent habits (food, activity, sleep, meds) lower risks and help you feel better.
- Your clinician will set personal blood glucose and A1C targets.
You won’t find a cure, but consistent habits lower risks and help you feel better. Your provider will set specific blood glucose and A1C targets to guide care as your condition changes.
Recognizing symptoms of type 2 diabetes early
Early signals from your body often point to rising blood sugar levels.
Many people have mild or no signs at first. Still, acting on common symptoms helps you get testing sooner and start treatment if needed.
Common signs to watch
- Increased thirst and frequent urination—these can mean your blood is high in sugar.
- Ongoing fatigue or blurred vision when glucose stays elevated.
- Hunger with weight loss or recurring infections that won’t clear.
Subtle changes that matter
- Tingling or numbness in your feet or hands and slow-healing sores on skin or feet.
- Dark, velvety patches on the neck or underarms (acanthosis nigricans) that may signal insulin resistance.
- Track patterns and share specifics with your provider to speed diagnosis of this condition.
| Symptom | Why it happens | What to do |
|---|---|---|
| Thirst, urination | High blood draws fluid from tissues | Check glucose and call your provider |
| Numbness, sores | Nerve, circulation problems | Inspect feet daily; seek care for wounds |
| Skin changes | Insulin resistance shows on skin | Note location and report at visit |
What causes insulin resistance and high blood sugar?
Understanding the root causes helps you see why early action matters.
When your cells stop responding to insulin, glucose can build up in the blood and raise fasting and after-meal levels. This process—called insulin resistance—often begins years before you notice a problem.
From genes to metabolism: how organs and cells play a role
Multiple factors combine to create resistance and rising blood sugar. Some are inherited: genes affect how your pancreas and cells make and use the hormone insulin.
Excess weight and metabolic syndrome worsen the problem. High blood pressure, raised triglycerides, and excess central fat change how cells respond and force the pancreas to overwork.
- Your cells become less responsive to insulin, so the pancreas pumps out more to hold glucose steady.
- The liver can release too much glucose between meals or overnight, raising fasting blood levels.
- Cell signaling can misfire, and beta cells eventually tire, lowering insulin output over time.
“Addressing these factors early slows progression and helps guide whether diet, activity, or medications are best.”
Knowing the mechanism directs treatment: lifestyle changes target weight and cell response, while some drugs act on liver output or preserve beta cell function. That combination helps keep blood sugar in safer ranges.
Who’s at higher risk of developing type 2 diabetes?
Knowing who faces greater risk helps you get screened earlier and act with purpose.
Some people carry higher odds due to age, family history, or pregnancy events. If you are 45 or older, have a parent or sibling with the condition, or had gestational diabetes—or delivered a baby over 9 pounds—you have a higher chance of developing it.
Age, family, ancestry, and pregnancy
Certain ancestries—Black or African American, Hispanic/Latino, American Indian, Asian American, and Pacific Islander—face greater risk. Ask your provider about earlier screening if you have these factors or a history of prediabetes.
Weight, inactivity, blood pressure, cholesterol, and PCOS
Overweight and central obesity raise insulin resistance. Physical inactivity, low HDL, high triglycerides, and high blood pressure increase the chance of progression to full disease.
- PCOS and depression also link to higher risk and may call for targeted tests.
- Prediabetes signals an opportunity to lower risk through diet, activity, and weight loss.
Talk to your clinician about when to test and which lifestyle changes address your personal factors. Small steps now can reduce future risk and protect heart and kidney health.

How type 2 diabetes is diagnosed today
Diagnosis starts with tests that clarify how your body manages sugar.
A1C shows your average glucose over the past 2–3 months and guides long-term care. A fasting plasma glucose is drawn after at least eight hours without food to spot higher morning values. A random plasma glucose may be checked immediately when you have clear symptoms.
A1C, fasting, and random checks
These labs answer different questions. A1C reflects longer trends. Fasting and random tests measure current blood sugar on the day of sampling.
Oral glucose tolerance testing
The OGTT measures glucose before and two hours after you drink a sweet solution. Your provider orders it when results are unclear or when pregnancy or borderline risk is a concern.
Understanding the stages
Care tracks a spectrum from insulin resistance to prediabetes, then to diagnosed disease and possible vascular complications. Typical A1C thresholds help classify each stage and shape treatment plans.
| Test | When used | What it shows |
|---|---|---|
| A1C | Routine screening and follow-up | Average glucose over 2–3 months |
| Fasting plasma glucose | After 8+ hours without food | Baseline morning blood sugar |
| OGTT | Unclear results or pregnancy screening | How your body handles a sugar load |
- Prepare: follow fasting instructions and report medicines before labs.
- Follow-up: testing frequency changes as your plan evolves.
- Ask: how results affect targets and next steps if your condition changes.
Blood sugar targets and daily monitoring strategies
Monitoring your glucose at home helps you spot trends and fine-tune daily choices.
Choosing a meter or a CGM depends on cost, access, how often you need readings, and whether you use insulin. A meter gives spot checks and is affordable. A CGM shows continuous data and trend arrows that help time meals and activity.
How often to test
If you use insulin, check more often around meals, at bedtime, and with symptoms. If you take oral or injectable meds and your plan is stable, fewer daily checks may be enough. Ask your provider for a schedule that fits your care plan.
Using patterns to guide actions
Record readings with context—meals, workouts, sleep, and stress—to find patterns. Use CGM time-in-range and trend arrows to shift meal timing or activity. Carry fast-acting carbs and a plan for lows or highs.
| Option | Best for | Pros | Cons |
|---|---|---|---|
| Glucose meter | Spot checking | Low cost, wide availability | Needs finger sticks, fewer trends |
| Continuous glucose monitor | Frequent insight, insulin users | Trend arrows, time-in-range reports | Higher cost, insurance limits |
| Combined use | Confirm CGM readings | Accuracy checks, backup | More supplies to manage |
| Log + share | All care plans | Better pattern detection, team review | Requires regular entries or app use |
Your type 2 diabetes diet: building meals that stabilize blood glucose
A reliable meal plan uses familiar foods to smooth your glucose and support steady energy all day.
Core groups: Base plates on lean protein—chicken, eggs, fish, or turkey—and plenty of non-starchy vegetables like broccoli, green beans, salad greens, and cucumbers.
Add healthy fats such as avocado, nuts, natural peanut butter, or olive oil to slow digestion and reduce spikes.
Carb quality and portion control
Choose complex carbs—beans, berries, sweet potatoes, whole-wheat bread—and boost fiber to slow carbohydrate absorption and steady blood sugar.
Use simple portion rules: a fist of carbs, a palm of protein, and two handfuls of vegetables per meal. This helps manage carbs without counting every gram.
Meal timing and meds
Eat regular meals and snacks to match your insulin or other medicines. Consistent timing helps prevent lows and limits large post-meal rises.
Foods to limit and practical tips
- Avoid refined grains, added sugars, and ultra-processed snacks that raise glucose quickly.
- Stay hydrated, include protein at breakfast, and plan snacks to bridge long gaps.
- Shop with a short list, read labels for added sugars, and swap sugary drinks for water or unsweetened tea to protect long-term treatment goals.
Exercise for type 2 diabetes: safer, smarter movement
Small, steady activity sessions can cut glucose spikes and boost daily energy.
Weekly goals: aerobic minutes and strength basics
Aim for at least 150 minutes per week of moderate aerobic activity, spread across most days. Add 2–3 sessions of strength work to build muscle and improve insulin sensitivity.

Pre-, during-, and post-workout tips if you use insulin
Talk with your provider before starting. If you use insulin, check blood before activity and carry quick carbs for lows.
During long or intense sessions, test again and adjust snacks or insulin per your plan. After exercise, monitor readings for delayed lows and have a recovery snack if needed.
How activity supports weight, blood pressure, and mood
Regular movement burns calories and trims waist size, helping with weight goals. It also improves blood pressure, circulation, and overall health.
Exercise boosts energy and eases stress, which makes sticking with healthy routines easier over time.
- Schedule brief walks or bike rides to reach 150 minutes weekly.
- Use resistance bands or bodyweight moves for strength at home.
- Check feet and wear proper shoes to prevent blisters and injury.
- Build habits by setting cues, tracking progress, and stacking activity onto daily chores.
Weight management and metabolic surgery options
Even a small drop on the scale often leads to measurable gains in blood sugar control.
Losing 5–7% of your body weight lowers fasting and post-meal glucose by improving insulin sensitivity and reducing resistance in muscle and liver cells.
Practical steps to reach modest weight loss
- Use portion control, boost fiber, and add lean protein each meal.
- Include regular strength training to preserve muscle while you lose weight.
- Track body measurements and non-scale wins like energy and sleep.
When surgery may be an option
For some with obesity and hard-to-control sugar, bariatric procedures offer greater weight loss and metabolic benefit than lifestyle alone.
“Surgery is a tool, not a cure; lifelong nutrition, follow-up, and support are essential.”
| Approach | How it helps | Benefits | Considerations |
|---|---|---|---|
| Modest weight loss (5–7%) | Improves insulin action | Lower fasting/post-meal glucose | Requires diet, activity, behavior change |
| Bariatric surgery | Limits intake or absorption | Larger, faster weight loss; can improve sugar control | Requires lifelong supplements and follow-up |
| Long-term care | Ongoing monitoring | Maintain results, prevent nutrient gaps | Insurance, candidacy, and surgical risks |
Prepare for consultations by documenting prior attempts, medications, and insurance coverage. Discuss risks, expected benefits, and long-term treatment plans with your team before deciding.
Type 2 diabetes medications: what to know
Medicines for managing blood sugar come in many forms, and each plays a different role in your care.
Oral first-line — metformin lowers liver glucose output and is often the starting treatment because it works well, is low cost, and has few serious side effects. Other pills include sulfonylureas, meglitinides, thiazolidinediones (TZDs), DPP-4 inhibitors, alpha-glucosidase inhibitors, and SGLT2 inhibitors.
Injectables — GLP-1 receptor agonists and the newer GIP/GLP-1 agent (tirzepatide) help control glucose and often reduce weight. They slow gastric emptying and lower appetite.
Insulin options include long-acting basal insulins (glargine, detemir), rapid-acting mealtime shots, pumps for continuous delivery, and inhaled insulin for some quick needs.
| Class | Main effect | When used | Notes |
|---|---|---|---|
| Metformin | Reduces liver glucose | First-line, most people | Low cost; GI side effects |
| SGLT2 | Increases urinary glucose loss | Cardio/renal benefit; weight loss | Watch for genital infections |
| GLP-1 / GIP-GLP-1 | Lower glucose, reduce appetite | When weight loss helpful | Injectable; nausea common |
| Insulin | Directly lowers blood sugar | When other meds insufficient | Hypoglycemia risk; dosing needs |
Combination therapy is common. Cost, side effects, and your goals guide choices. Also treat high blood pressure and cholesterol to cut heart and kidney risks.
Managing high blood pressure and cholesterol with diabetes
Controlling blood pressure and cholesterol is as important as managing your glucose to prevent heart and vessel harm.
Setting targets to protect your heart and blood vessels
Keeping blood pressure and cholesterol near goal levels lowers the chance of heart attack and stroke. Your clinician will set individual targets based on age, kidney function, and overall risk.
Regular screening helps you catch rising numbers early and adjust treatment before damage develops.
Lifestyle plus medication to lower overall cardiovascular risk
Dietary fiber, limiting sodium, regular activity, and modest weight loss all improve blood and cholesterol markers. Quitting tobacco and improving sleep also reduce cardiovascular risk.
Many people need medicines in addition to lifestyle changes. Common options include statins for cholesterol and ACE inhibitors or ARBs for blood pressure. These drugs lower risk beyond what lifestyle alone provides.
- Why goals matter: they protect your heart and vessels over years.
- Practical steps: high-fiber foods, less salt, regular walks, and weight control.
- Medications: ask about statins, blood pressure agents, and how they interact with your current plan.
- Monitoring: check blood pressure at home and bring readings to visits for timely adjustments.
- Coordination: align care among your primary clinician, pharmacy, and specialists to reduce side effects and gaps.
| Measure | Common target | Why it matters |
|---|---|---|
| Blood pressure | <130/80 mmHg | Lower risk of stroke, heart attack, and kidney harm |
| LDL cholesterol | Varies by risk: often <70–100 mg/dL | Reduces artery plaque and heart events |
Preventing complications: protecting your heart, kidneys, eyes, nerves, and skin
Keeping your blood levels steady protects more than glucose—it guards your heart, eyes, kidneys, nerves, and skin.
Heart disease and stroke: how damage develops and what you can do
High blood raises the risk of atherosclerosis, angina, heart attack, and stroke. Over time, arteries narrow and block blood flow.
Lowering blood pressure, controlling cholesterol, and steady glucose control cut that risk. Seek care for chest pain, unusual shortness of breath, or sudden numbness—these are urgent signs.
Kidney and eye screening: early checks that save function
Early kidney problems show as albumin in the urine or a falling eGFR. Annual urine albumin and periodic eGFR tests help detect trouble early.
Get a dilated eye exam at least once a year or as your provider recommends to spot retinopathy before vision drops.
Nerve health and foot care: daily checks prevent ulcers
Neuropathy causes numbness and loss of feeling in your feet. Check feet daily for cuts, blisters, or redness.
Wear supportive shoes, trim toenails carefully, and see a podiatrist for calluses or persistent sores to avoid infection and ulcers.
Skin and wound care: protect circulation and speed healing
Dry skin and slow-healing wounds raise infection risk. Moisturize gently, avoid harsh chemicals, and inspect minor wounds daily.
Call your provider for wounds that grow, drain, or do not start to heal within a few days.
| Check | How often | Why it matters | When to call |
|---|---|---|---|
| Blood pressure & cholesterol | Every 3–12 months | Reduces heart and stroke risk | Sudden chest pain or very high readings |
| Urine albumin / eGFR | Annually | Finds early kidney damage | Reduced urine output or swelling |
| Dilated eye exam | Annually | Detects early retinopathy | New vision changes or flashes |
| Foot and skin check | Daily at home; clinic yearly | Prevents ulcers and infections | Open wound, redness, or numbness |
Keep a simple checklist in your phone or binder with these visits and test dates. Consistent control plus routine screening are your best defense against long-term problems from this condition.
Daily self-care routines that make managing diabetes easier
A short, consistent checklist each morning and evening supports safer control.
Foot checks, dental and eye visits, and regular physicals
Do a quick foot check every day. Look for cuts, redness, or swelling on your feet and between toes. Treat issues early and call your clinician if a wound looks infected.
Schedule an annual eye exam and cleanings with your dentist. Get a full physical each year to review medications and labs.
Sleep, alcohol, and a sick day plan to keep levels steady
Aim for at least seven hours of sleep nightly. Poor sleep raises blood sugar and makes stress harder to handle.
If you drink alcohol, do so carefully. Alcohol can lower or raise glucose; check levels more often when you drink and eat a snack if needed.
Have a written sick day plan: increase testing, keep oral fluids, and know when to hold or adjust medicines. Even a mild illness can change your needs.
When to call your care team and adjust your plan
Call your team if you have repeated high readings, fever, vomiting, or a wound that won’t heal. Emergency signs include very low blood or sudden breathlessness.
| Action | When | Why |
|---|---|---|
| Foot check | Daily | Spot infections early to avoid complications |
| Eye/dental visit | Annually | Detect changes before they affect vision or oral health |
| Sleep goal | Nightly | Improves glucose control and mood |
| Sick day plan | As needed | Keep levels stable and avoid hospital visits |
Quick checklist: daily feet review, medication check, test blood as directed, and keep supplies organized for home and travel. Small routines add up and help you stay on track with your care and condition.
Mental health, stress, and diabetes distress
Mental strain can make daily self-care feel heavier than it should.
People with chronic glucose problems are about 2–3 times more likely to have depression and roughly 20% more likely to have anxiety. That emotional load—often called diabetes distress—can lead you to skip tests, miss meals, or stop medicines.
Spotting depression and anxiety—and getting help
Watch for persistent low mood, lack of interest, worry that interferes with sleep or tasks, and declining motivation to follow your plan. Talk with your provider early; therapy and medication can restore function and safety.
Stress management, support groups, and mind-body practices
Practical tools work: breathing exercises, short walks, gentle yoga, meditation, journaling, and peer groups. These lower stress, boost energy, and help you stick with healthy choices and medicines.
| Problem | Sign | Action |
|---|---|---|
| Depression | Loss of interest, low mood | Seek therapy; consider medication with your clinician |
| Anxiety | Persistent worry, sleep trouble | Try CBT, relaxation techniques, and talk to your provider |
| Diabetes distress | Burnout, skipping self-care | Join support groups; use small daily routines and involve loved ones |
- You’ll learn signs that warrant a conversation with your care team.
- You’ll get coping tools to lower stress and protect adherence.
- You’ll see how better mental health boosts energy and health outcomes.
Access, equity, and the cost of type 2 diabetes in the United States
Costs and access shape who gets timely care and which medicines reach people in different communities.
Disparities in diagnosis and medication access
Rates are higher among Latino (12%), Black (12%), and Asian (10%) populations, and about 14.5% in American Indian communities, versus 7% in white people.
Minority groups are less likely to receive newer medicines and are underrepresented in clinical trials, which raises long-term equity concerns and adds to outcome gaps.
Budgeting for care: devices, visits, and insurance tips
Annual medical spending averages $19,736 per person, with $12,022 directly related to diabetes care.
About 15% live in poverty, 19% face food access problems, and 51% report low-quality diets—factors that raise risk and complicate management.
- Check your plan’s formulary and ask about prior authorization or patient assistance programs.
- Use community clinics, discounted lab programs, and nutrition supports to lower bills.
- Discuss cost openly with your clinician to find effective, affordable regimens.
- Seek trial opportunities to improve inclusion and access to newer therapies.
| Expense | Typical annual amount | Notes |
|---|---|---|
| All medical costs | $19,736 | Average per person |
| Direct condition costs | $12,022 | Supplies, meds, visits |
| Food/access concerns | 19% | May affect outcomes |
Supplements, alternative therapies, and product claims: HepatoBurn Review
Before you try a new supplement for glucose or weight, learn what research actually shows.
What studies say about common supplements
Chromium has been tested in many trials. Most show little or no lasting benefit and high doses can cause harm.
Cinnamon may lower fasting glucose a little, but it does not reliably change long-term A1C results.
Magnesium findings are mixed; some people see modest gains, while excess intake risks stomach upset and dangerous blood levels.
HepatoBurn and similar weight-loss aids: safety and red flags
- Claims: rapid fat loss, detox, or appetite shutdown often lack peer-reviewed evidence.
- Red flags: proprietary blends, stimulant combos, unclear doses, and “detox” marketing.
- Regulation: most supplements are not FDA-approved for safety or efficacy and can be contaminated or inconsistent.
Interactions and why they aren’t a substitute for prescribed care
Supplements can change how your medications work, especially glucose-lowering, blood pressure, or cholesterol drugs. That raises risk for lows, high readings, or side effects.
Use them only after discussing with your provider. Maintain prescribed treatment and proven lifestyle steps—diet, activity, and meds—since supplements do not replace standard treatment and monitoring.
Quick vetting tips: look for third-party testing, published studies, clear ingredient amounts, and a plan with your clinician to stop if problems arise.
type 2 diabetes: putting your plan into action today
Begin with a short, clear plan that links meals, movement, and monitoring.
Start each day with a simple routine: breakfast with protein, a brief walk, and a scheduled check of your blood sugar. Aim for pre-meal targets your clinician set and test before and about two hours after larger meals or workouts to track trends.
Two easy meal changes you can try: swap sugary drinks for water or unsweetened tea, and add a palm-sized protein at breakfast. One activity goal to start this week: three 10-minute walks spread across the day.
Create a medication checklist and set phone alarms or a pillbox reminder. Schedule follow-up labs and a visit in 3 months to review numbers and adjust treatment as needed.
Pack a backup kit for travel or minor illness: testing supplies, fast carbs, meds, and a short action plan. Pick one stress habit—deep breathing for five minutes daily—to support consistency.
Share your plan with one support person so you’re not managing this alone. Regular follow-up and steady habits make better long-term care and steadier levels more likely.
Conclusion
Conclusion
This condition is lifelong but manageable — and small changes make a big difference.
You can lower A1C, reduce risk, and add years of better health by quitting smoking, keeping routine monitoring, and following proven lifestyle and medication plans. Regular checks of blood and timely screenings catch problems early so interventions work best.
Pair daily habits—meal choices, movement, sleep, and stress skills—with devices and meds as your team advises. Watch for unsupported product claims and discuss any supplement before use.
Next step: pick one action from this guide today, tell a support person, and set a short follow-up with your clinician to keep momentum and protect long-term well‑being.
FAQ
What are the earliest signs you should watch for?
Early signals include increased thirst, needing to urinate more often, persistent fatigue, and blurred vision. You may also notice slow-healing cuts, numbness or tingling in your feet, recurring infections, or unexplained weight loss. If you experience any of these, ask your clinician for glucose testing and an A1C check.
How does insulin resistance lead to high blood glucose?
Insulin helps your cells absorb sugar for energy. When cells resist insulin’s signal, the liver keeps releasing glucose and your pancreas overworks beta cells. That raises blood sugar and, over time, leads to sustained high levels and metabolic strain unless you change diet, activity, or start medication.
Who is more likely to develop this condition?
Risk rises with older age, family history, and certain ethnic backgrounds. Excess weight, physical inactivity, high blood pressure, abnormal cholesterol, and conditions like polycystic ovary syndrome (PCOS) or pregnancy-related elevated sugar also increase risk.
Which tests confirm a diagnosis and what do they mean?
Common tests are the A1C, fasting plasma glucose, and random glucose. An oral glucose tolerance test may be used for borderline cases. These tests determine whether you have insulin resistance, prediabetes, or established disease and guide treatment choices.
What blood sugar targets should you aim for daily?
Targets vary by age, health status, and treatment. Typical goals might include premeal and bedtime ranges advised by your care team. Monitoring with a glucose meter or continuous glucose monitor (CGM) helps you see trends and adjust food, activity, or medication safely.
How should you plan meals to stabilize blood sugar?
Build meals around lean protein, non-starchy vegetables, healthy fats, and complex carbohydrates. Focus on fiber and portion control, limit refined grains and added sugars, and time meals and snacks to match any insulin or medication schedule to avoid highs and lows.
What exercise routine is safe and effective for managing glucose and weight?
Aim for regular aerobic activity plus two or more days of strength training weekly. If you use insulin, monitor your levels before, during, and after workouts and carry fast-acting carbs. Exercise helps lower blood pressure, improve cholesterol, and support weight loss.
When should you consider weight-loss surgery?
Losing 5–7% of body weight can improve insulin sensitivity. Bariatric surgery becomes an option if lifestyle changes and medications don’t control weight or glucose and if your clinician determines you meet criteria. It requires long-term follow-up and lifestyle commitment.
What medication options exist and how are they chosen?
Treatment can include metformin and other oral medicines, injectable GLP-1 agonists or dual GIP/GLP-1 drugs, and insulin for some people. Choice depends on glucose levels, weight goals, side effects, cost, and other conditions like high blood pressure or cholesterol.
How do you manage blood pressure and cholesterol with this condition?
Set targets with your clinician to lower cardiovascular risk. Lifestyle changes—diet, activity, and weight loss—help, and many people need medications such as ACE inhibitors, ARBs, statins, or other agents to protect heart and kidney health.
What steps prevent complications to heart, kidneys, eyes, nerves, and skin?
Regular screenings—A1C, blood pressure checks, kidney tests, eye exams, and foot inspections—catch problems early. Control glucose and blood pressure, quit smoking, manage cholesterol, and treat wounds promptly to reduce the risk of heart attack, stroke, kidney disease, vision loss, and ulcers.
What daily self-care should you practice?
Do daily foot checks, keep up dental and eye visits, get regular physicals, maintain healthy sleep and alcohol habits, and have a sick day plan. Know when to call your care team—markedly high or low glucose, fever, or signs of infection require prompt attention.
How does stress affect blood sugar and what can you do about it?
Stress and mood disorders can raise glucose through hormonal pathways and affect self-care. Use stress reduction strategies, seek counseling or support groups, and talk to your provider if you face depression or anxiety that interferes with management.
Are supplements like chromium or cinnamon helpful, and what about weight-loss products?
Some supplements show limited evidence for small benefits, but results vary and quality is inconsistent. Weight-loss aids like HepatoBurn lack robust, reliable evidence and may pose safety risks. Always consult your provider before adding supplements; they do not replace proven treatments.
How do cost and access affect long-term care in the United States?
Medication, devices, and regular visits can be expensive and access varies by insurance and community. Discuss generic options, patient assistance programs, and diabetes education resources with your care team to reduce financial barriers and improve outcomes.
What immediate actions can you take today to improve your health?
Start by checking your risk factors, scheduling screening tests if needed, improving meal choices, increasing daily activity, and talking with your clinician about a personalized plan. Small, consistent changes lower glucose, blood pressure, and long-term complication risk.
