If you’ve been searching for how to detox your liver for fat loss, you’re not alone — when the scale barely moves and health feels fragile, the right approach can bring both clarity and lasting results.
The liver performs over 500 vital tasks that keep the body steady: filtering toxins like alcohol and medications, storing vitamins, and helping manage blood sugar. Many marketed cleanses claim dramatic results, yet research shows they often lack FDA oversight and clinical proof.
We define a safe way that supports natural processes rather than chasing shortcuts. Later, we will review HepatoBurn and weigh claims against evidence, risks, and our recommendation.
This guide is for people at risk of disease or those seeking steady weight loss. We will debunk myths, outline sensible lifestyle ways, and set realistic expectations for lasting change.

Key Takeaways
- Support natural liver function instead of relying on unproven cleanses.
- Sustainable weight loss depends on daily habits, not single products.
- Many detox products lack regulation and can harm the organ.
- We will review HepatoBurn with evidence-based criteria.
- Seek medical care if you have risk factors for liver disease.
Why liver health matters for weight loss right now
Liver function sits at the crossroads of nutrient handling and bodyweight control. The organ filters alcohol, medications, and waste while processing nutrients and regulating blood sugar. This work shapes appetite, energy, and how the body stores or burns fat.
Long-term alcohol use, obesity, insulin resistance, viral hepatitis, environmental toxins, genetics, and excess medications or supplements can impair liver function. Those factors raise the chance of liver disease and fatty liver disease, which often slows weight progress.
Modest, steady changes in diet and activity can de-fat the liver over time. Maintaining a BMI in the 18–25 range lowers risk. Men should aim for no more than three drinks per day and women no more than two to cut added calories and organ workload.
| Driver | Why it matters | Practical step |
|---|---|---|
| Alcohol | Adds calories and increases liver workload | Limit intake; follow daily drink guidance |
| Obesity / insulin resistance | Promotes fatty liver and metabolic disease | Focus on steady weight change and balanced diet |
| Hepatitis & toxins | Can cause chronic damage and reduced function | Screen when at risk; reduce exposures |
| Medications / supplements | Overuse may harm liver cells | Review meds with a clinician |
Debunking liver detox myths with current evidence
Many marketing messages promise quick fixes, but the evidence rarely matches the claims. We examine common myths and pair each one with current research and practical steps.
Myth: Cleanses are necessary for daily maintenance
The healthy liver already performs continuous filtering and metabolic work. Cleanses marketed for daily upkeep are not regulated by the FDA and lack uniform standards.
Clinical trials are scarce, and routine use of those products is not supported by robust human data.
Myth: Products help you lose weight
There is no high-quality research showing that marketed products accelerate weight change. Some ingredients, like milk thistle or turmeric, show biological signals in preliminary studies, but they are not proven for routine prevention or weight effect.
Unregulated supplements can cause drug-induced liver injury, producing the very liver damage they claim to prevent.
Myth: You can’t prevent liver disease or reverse damage
Prevention is possible. Moderating alcohol, keeping a healthy BMI, avoiding risky exposures, and screening when indicated reduce risk of fatty liver disease and other problems.
People can reverse certain conditions: weight loss improves fatty liver, stopping alcohol helps alcoholic liver disease, and modern treatments exist for viral hepatitis.
“Small, consistent lifestyle changes outperform short-term products for both liver metrics and lasting weight outcomes.”
- Most cleanses lack FDA oversight and solid clinical data.
- Supplements can interact with medications; always talk doctor before starting them.
- Focus on prevention and evidence-based treatments rather than marketing claims.
| Claim | Evidence | Practical note |
|---|---|---|
| Cleanses restore daily function | No uniform regulation; limited clinical support | Rely on healthy habits instead |
| Products produce rapid weight change | No high-quality trials showing weight effects | Use proven weight strategies for fatty liver |
| Supplements are always safe | Reported cases of drug-induced liver injury exist | Discuss supplements with a doctor, especially with meds |
| Liver disease cannot be prevented or treated | Evidence supports prevention and effective therapies | Screen when at risk; pursue medical treatments if needed |
How to detox your liver for fat loss the safe, science-backed way
We favor steady, evidence-based steps over quick promises. This way protects organ function while you lose weight at a reasonable pace.
Set realistic goals: slow, steady weight loss protects your liver
Aim for about 1–2 pounds per week. For NAFLD, losing 3–5% of body weight reduces liver fat; 7–10% gives greater improvement. Rapid drops can stress metabolism and raise risk.
Focus on daily habits over quick fixes or detox products
Build a lifestyle of balanced meals, regular movement, hydration, and sleep. Start with consistent meals and short daily walks, then layer in alcohol moderation and medication review.
Work with your doctor if you have symptoms or conditions
We urge you to talk doctor before major changes, especially with multiple prescriptions or metabolic disease. No medication reliably “cleans” fatty liver; clinical research supports gradual treatment and monitoring.
“Small, steady changes deliver measurable liver benefits and sustainable weight outcomes.”
- Track weekly metrics: steps, meal plans, alcohol-free days.
- Sequence efforts: meals and movement across the day, then medication checks.
- Address multiple levers at once—diet, alcohol, activity—rather than one product.
Eat and drink for liver health: what to choose, what to limit
What we eat and sip each day sets the stage for long-term liver improvement and metabolic health.
A Mediterranean-style pattern—leafy greens, berries, beans, whole grains, fish, and lean proteins—supports fatty liver disease improvement and steady weight change. Aim for gradual progress: about 1–2 pounds weekly and a 3–5% body weight drop for early liver benefit.
Mediterranean-style choices
Make plants and whole grains the base. Build meals around colorful vegetables, berries, legumes, and oats. Include fish, poultry, yogurt, tofu, or beans for protein that avoids excess saturated fat.
Fat quality matters
Replace saturated and trans fats with unsaturated options: extra-virgin olive oil, nuts, seeds, avocados, and omega-3 rich fish. These swaps improve blood lipids and support better markers of liver health.
Cut added sugar and refined carbs
Limit sugar-sweetened drinks and packaged sweets because excess fructose and refined carbs raise liver fat. Read labels and choose whole foods when possible.
Hydration targets
Aim for at least 64 ounces of water daily, unless your clinician advises otherwise. Practical tips: carry a 20-oz bottle, sip between meals, and include water-rich foods like cucumbers and melons.
“Sustained food and drink changes, not single products, deliver measurable benefits for people with fatty liver disease.”
- Shop a color-rich produce list and batch-cook grains and legumes.
- Keep olive oil, nuts, and seeds as default cooking and snack fats.
- Use label-reading to spot added sugar and industrial trans fats.
Practical planning and steady habits compound with activity changes to reduce fatty liver over time and protect overall health.
Alcohol, medications, and supplements: lower your liver risk
We recommend simple safety steps that protect organ function and support steady progress. Managing alcohol and medicines reduces the chance of disease and drug-related damage while keeping weight goals realistic.
Limit alcohol or abstain based on risk
Men: no more than three drinks per day; women: no more than two. People with alcoholic liver disease need complete abstinence so healing can begin.
Practical moves: add alcohol-free days, pace drinks with water, and choose satisfying nonalcoholic options for social situations.
Use medications wisely and be cautious with supplements
Avoid exceeding labeled doses, watch acetaminophen totals, and be careful with cold or combo remedies. Overuse of common meds is a known source of organ injury.
Unregulated supplements may contain multiple active compounds at unclear doses and can cause harm. We recommend a medication and supplement audit with your doctor to spot interactions and side effects.
- Read labels: avoid stacking products with the same ingredients.
- Watch for warning signs: jaundice, dark urine, or increasing abdominal pain—seek care promptly.
- Prefer proven treatments: discuss safer, evidence-based options rather than relying on unverified blends.
“We will use these safety principles when evaluating HepatoBurn and similar products later.”
Move more to reduce fatty liver and support weight loss
Movement is a powerful, low-risk medicine. Regular activity lowers inflammation and improves insulin sensitivity, two key drivers of liver health and steady weight change.
Aerobic and resistance training: weekly time and intensity targets
Aim for more than 200 minutes per week of moderate exercise, split across 4–7 days. Sessions of 20–60 minutes are effective and manageable.
Pair brisk walking, cycling, or swimming with strength work—bodyweight, bands, or weights—three times weekly. This combo lowers inflammation and protects lean mass.
Research shows diet plus exercise induced remission in many people with fatty liver disease. That evidence supports making movement a central part of care.
Build a sustainable routine: from sedentary to active safely
Start small if you sit most of the day: begin with 10–15 minutes daily and add five minutes each week. Gradual progress cuts injury risk and builds confidence.
- Track steps or active minutes so gains are visible and motivating.
- Use practical sequences: brief walks after meals and short strength circuits on alternate days.
- Include low-impact options and planned recovery days to preserve momentum.
Expect better energy, clearer appetite signals, and steady weight change within weeks when movement pairs with sensible eating. These effects compound over months and support lasting disease improvement.
HepatoBurn Review: claims, evidence, and our recommendation
We reviewed HepatoBurn’s claims against clinical evidence and safety signals. Below we summarize promises, the regulatory reality, and clear risks that matter for anyone considering a supplement.
What HepatoBurn promises
HepatoBurn often promises faster weight change, improved liver health, and toxin flushing through proprietary herbal blends and extracts. Marketing typically highlights rapid results and natural ingredients.

What research and regulation show
Detox-style products are not FDA-approved for safety or efficacy. Ingredient quality and doses vary between batches. Published research does not show these products outperform diet and exercise for lowering organ fat or treating liver disease.
Potential risks and side effects
Multi-ingredient formulas raise the chance of interactions and unpredictable side effects. Some supplements have been linked to drug-induced organ damage in case reports.
- Certain botanicals (milk thistle, turmeric) show biological signals in small studies but lack robust human trials for routine treatment.
- Combining unregulated blends with prescription drugs can alter absorption or metabolism and increase risk.
- Stop use and seek care if you notice jaundice, dark urine, worsening abdominal pain, or severe fatigue.
Our verdict
We recommend prioritizing proven treatments and steady habits over HepatoBurn. Diet, activity, alcohol moderation, hydration, and clinician-guided care deliver safer, measurable benefits with far less risk.
“If you still consider a supplement, discuss it with a clinician who can assess interactions, monitoring, and individual risk.”
Know the signs, risks, and when to talk to your doctor
Watch for early warning signs so problems can be treated before they worsen.
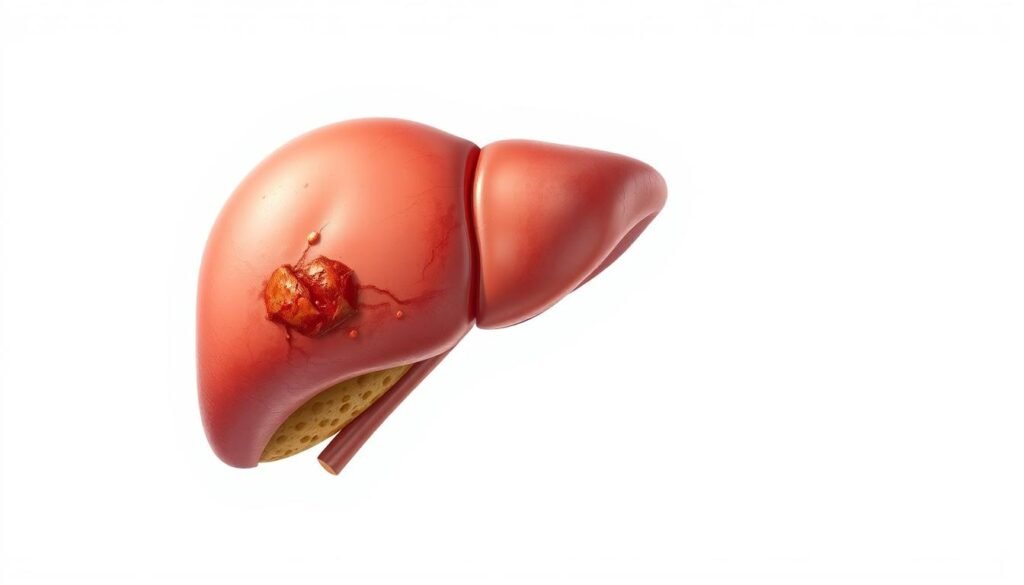
Early symptoms you shouldn’t ignore
Unusual fatigue, appetite loss, or persistent nausea can signal that the organ is under stress.
Also watch for pale stools or dark urine, yellowing of the skin or eyes (jaundice), swelling in the abdomen or legs, itchy skin, and easy bruising.
These signs reflect slowing processing and may indicate liver damage or progressing liver disease. Prompt evaluation often prevents worse outcomes.
Major risk factors
Key risks include long-term alcohol use, excess weight and insulin resistance, viral hepatitis B or C, environmental toxins, certain genetic conditions, and overuse of some medications or supplements.
People with multiple conditions face higher odds of damage and should prioritize coordinated care.
Screening, vaccinations, and ongoing monitoring
Consider screening if you have risk factors or a family history. Doctors use blood tests and imaging like ultrasound to check for fatty liver and other problems.
Vaccination against hepatitis A and B is recommended if you are not immune. Effective oral treatments exist for chronic hepatitis B and C; early management improves outcomes.
- When to talk doctor urgently: jaundice, severe abdominal pain, confusion, or rapid swelling.
- When to schedule screening: persistent symptoms, known risk factors, or abnormal blood tests.
- Bring a checklist: symptom timeline, alcohol intake, full medication and supplement list.
“Early action, combined with alcohol moderation and weight care, gives the best chance of recovery.”

Conclusion
We close with a clear takeaway: simple, proven habits beat unregulated supplements when protecting the liver and managing disease risk.
Aim for steady change: losing about 7–10% of body weight helps de-fat the liver, and extreme measures often cause setbacks. No single medication clears fatty liver; lifestyle and targeted treatments deliver real effects.
Prioritize a Mediterranean-leaning diet, lower added sugar, better fat quality, and at least 64 ounces of water daily. Pair that with more than 200 minutes per week of mixed aerobic and strength work and alcohol moderation.
Skip risky detox blends. Review medications, get screened and vaccinated when needed, and work with clinicians on treatment choices. Pick one or two small changes this week—plan meals and schedule walks—and build steady progress for lasting health and weight goals.
FAQ
What role does liver health play in weight and metabolic health?
The liver regulates glucose, fat metabolism, and inflammation. When excess fat accumulates in liver cells, insulin resistance and systemic inflammation rise, which makes weight control harder. By improving liver function through diet, activity, and reduced alcohol use, we support metabolic health and make sustainable weight loss more achievable.
Are cleanses or detox products necessary for maintaining liver function?
No. The liver is designed to clear toxins and does this continuously. Evidence does not support routine cleanses. We recommend evidence-based lifestyle steps—balanced diet, regular exercise, weight management, and limiting alcohol—rather than short-term products that promise quick fixes.
Do supplements like HepatoBurn reliably reduce liver fat or cause weight loss?
Most over-the-counter formulas lack robust clinical proof and aren’t regulated like medications. Some ingredients may have theoretical benefit, but safety and efficacy vary. We advise prioritizing proven lifestyle changes and discussing any supplement with a clinician before use, especially if taking other medications.
How quickly should we aim to lose weight to protect the liver?
Slow, steady weight loss—about 1 to 2 pounds per week—is safest. Rapid loss risks gallstones and stress on the body. Even modest weight reduction (5–10% of body weight) can significantly reduce liver fat and improve lab markers over months.
Which eating pattern best supports liver health and reducing fatty liver?
Mediterranean-style eating—vegetables, fruits like berries, whole grains, legumes, lean proteins, and healthy fats such as olive oil and nuts—shows consistent benefits. It reduces liver fat, lowers inflammation, and supports long-term weight control.
How important is sugar and refined carb reduction for fatty liver?
Very important. Added sugars and refined carbohydrates increase liver fat and insulin resistance. Cutting sugary drinks, sweets, and ultra-processed grains helps lower liver fat and aids weight loss when combined with overall calorie control.
What alcohol limits should people with or at risk for fatty liver follow?
If we have diagnosed fatty liver or liver disease, abstaining from alcohol is often best. For those at lower risk, current guidance suggests limiting intake—generally no more than one drink per day for women and two for men—but individual recommendations depend on medical history, so we should consult our doctor.
Can medications or common supplements harm the liver?
Yes. Several prescription and over-the-counter drugs, plus some herbal supplements, can cause liver injury. We must use medications only as prescribed, inform providers about all supplements we take, and seek testing if symptoms like jaundice, dark urine, or severe fatigue appear.
What exercise dose is effective against fatty liver?
Both aerobic activity and resistance training help. Aim for at least 150 minutes of moderate aerobic exercise weekly plus two days of strength training, or the equivalent in vigorous activity. Consistency matters more than intensity; small increases from a sedentary baseline yield benefits.
When should we see a doctor or get screened for liver disease?
See a clinician if we have risk factors—obesity, type 2 diabetes, heavy alcohol use, or persistent abnormal liver blood tests—or symptoms like abdominal pain, jaundice, or unexplained fatigue. Screening tests may include liver enzymes, imaging, or specialist referral for diagnosis and monitoring.
Are there safe steps we can take at home to support liver recovery?
Yes. We can adopt a Mediterranean-style diet, reduce added sugars and refined carbs, increase physical activity, lose weight gradually, stay hydrated, limit alcohol, and avoid unnecessary supplements. These changes improve liver markers and overall health without relying on unproven products.
Can fatty liver be reversed, and what timeline is realistic?
In many cases, early-stage fatty liver (nonalcoholic fatty liver) is reversible with sustained lifestyle changes. Improvements in liver fat and function can appear within months of weight loss and exercise, but advanced fibrosis or cirrhosis may be only partially reversible and require specialist care.
What symptoms of liver injury should never be ignored?
Seek prompt medical attention for jaundice (yellowing of skin or eyes), dark urine, pale stools, severe abdominal pain, persistent nausea or vomiting, unexplained bleeding or bruising, or sudden extreme fatigue. These signs can indicate serious liver damage.
How do vaccinations and screening help reduce liver disease risk?
Vaccination against hepatitis A and B prevents viral causes of liver injury. Routine screening for viral hepatitis, alcohol counseling, and monitoring liver enzymes in high-risk individuals allow early detection and treatment, reducing progression to advanced disease.